Electrocution of TN MBBS student at Wayanad resort, owner arrested for neglecting earth leakage
The police have arrested the resort owner for allegedly ignoring warning about earth leakage from a steel fence around the pool.
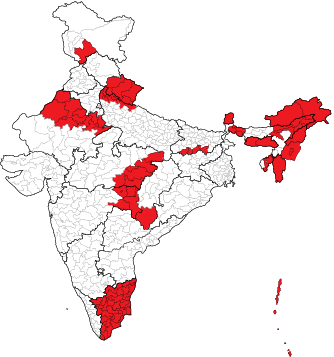
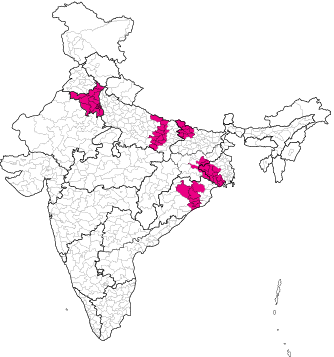
Phase 1 April 19
21 States
102 Constituencies
- Arunachal Pradesh (2)
- Assam (5)
- Bihar (4)
- Chhattisgarh (1)
- Madhya Pradesh (6)
- Maharashtra (5)
- Manipur (2)
- Meghalaya (2)
- Mizoram (1)
- Nagaland (1)
- Rajasthan (12)
- Sikkim (1)
- Tamil Nadu (39)
- Tripura (1)
- Uttar Pradesh (8)
- Uttarakhand (5)
- West Bengal (3)
- Andaman and Nicobar Islands (1)
- Jammu and Kashmir (1)
- Lakshadweep (1)
- Puducherry (1)
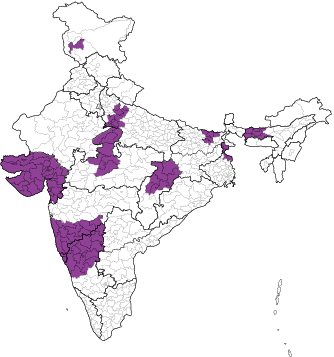
Phase 2 April 26
13 States
89 Constituencies
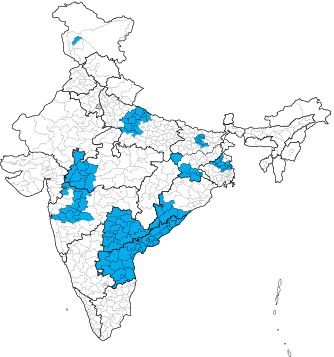
Phase 3 May 7
12 States
94 Constituencies
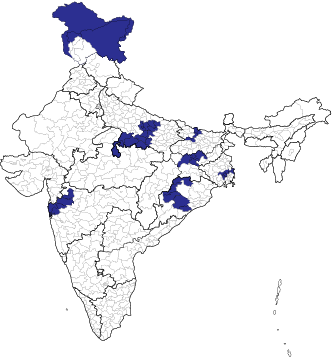
Phase 4 May 13
10 States
96 Constituencies
Phase 5 May 20
8 States
49 Constituencies
Phase 6 May 25
7 States
57 Constituencies
Phase 7 June 1
8 States
57 Constituencies
| Constituency | 2024 | 2019 |
|---|---|---|
| Thiruvananthapuram | 66.47% | 73.66% |
| Attingal | 69.48% | 74.4% |
| Kollam | 68.15% | 74.66% |
| Pathanamthitta | 63.37% | 74.24% |
| Mavelikkara | 65.95% | 74.23% |
| Alappuzha | 75.05% | 80.25% |
| Kottayam | 65.61% | 75.44% |
| Constituency | 2024 | 2019 |
|---|---|---|
| Idukki | 66.55% | 76.34% |
| Ernakulam | 68.29% | 77.63% |
| Chalakudy | 71.94% | 80.49% |
| Thrissur | 72.90% | 77.92% |
| Alathur | 73.42% | 80.42% |
| Palakkad | 73.57% | 77.72% |
| Ponnani | 69.34% | 74.98% |
| Constituency | 2024 | 2019 |
|---|---|---|
| Malappuram | 72.95% | 75.49% |
| Kozhikode | 75.52% | 81.65% |
| Wayanad | 73.57% | 80.33% |
| Vadakara | 78.41% | 82.67% |
| Kannur | 77.21% | 83.21% |
| Kasaragod | 76.04% | 80.65% |

































































































































.jpg.transform/170x160/image.jpg)




















